If the operation to remove the tonsils was frequently performed twenty years ago, it is much less systematic today. Indications, risks, side effects… The point with Dr. Patrick Aubé, general practitioner.
The removal of the tonsils also called “tonsillectomy” Where “tonsillectomy” can be decided when they obstruct the airways
What are the tonsils for?
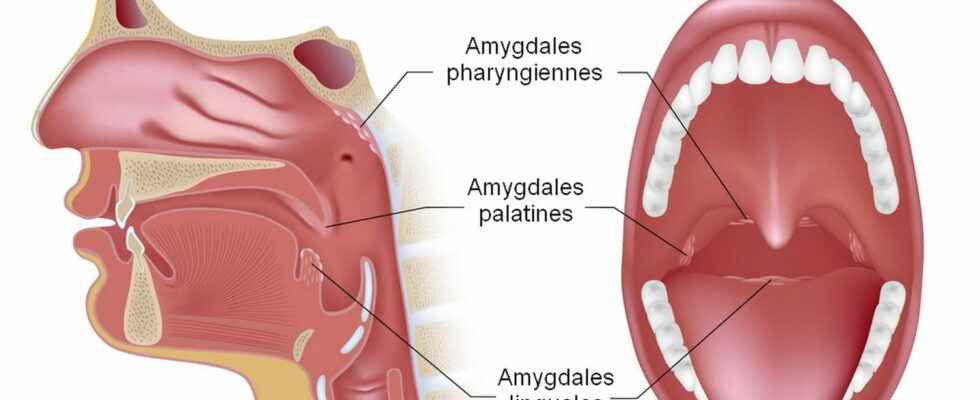
Tonsillectomy, sometimes called tonsillectomy, is the surgical removal of the tonsils. While it is true that the tonsils play an important role in immune defense, they can also obstruct the airways. It exists three types of tonsils: palatal and lingual (the ones you see) and the pharyngeal tonsils (vegetations). All are lymphoid organs of the larynx. Genuine body’s protective barriers, they oppose infections in the same way as lymph nodes do. In case of infection, the tonsils swell.
When should the tonsils be removed?
In children, tonsillectomy concerns the removal of the palatine tonsils in the event of repeated angina or chronic tonsillitis in particular. It is frequently associated with adenoidectomy where the pharyngeal tonsils or adenoids are removed. In young children (under 6 years old), the main indication ischronic respiratory obstruction related to enlarged tonsils. In 2020, the French Society of ENT and Face and Neck Surgery (SFORL) updated its recommendations regarding the removal of tonsils in children and clarified that tonsillectomy is not recommended for the treatment of simple snoring and she is not also not recommended for the treatment of recurrent angina or pharyngitis in children occurring at a frequency of less than 7 infectious episodes over the last year, or less than 5 episodes/year over the last 2 years, or less than 3 episodes per year over the last 3 years.
Overly large tonsils
Oversized tonsils prevent you from breathing properly and to swallow well, are often the indication for 80% of cases of tonsillectomy. It is then most often associated with an adenoidectomy, that is to say removal of the vegetations. The appearance ofsleep apnea caused by these too large tonsils is often also observed. When the tonsils are too big, they can indeed partially obstruct the airways, causing a snoring accompanied by pauses in breathing, with poor quality sleep. Children are tired all day, and may have school problems. On the other hand, exhausted, they are likely to eat less, especially if the tonsils sometimes interfere with swallowing, and to have growth retardation. Tonsillectomy then often has very positive consequences on the physical and psychological health of his children.
Repeated angina
20% of tonsillectomies are performed for angina or abscess. Recurrent angina is one of the main infectious indications. But the operation is not not recommended for the treatment of recurrent angina or pharyngitis in children occurring at a frequency of less than 7 infectious episodes over the last year, or of less than 5 episodes/year over the last 2 years, or of less than 3 episodes per year over the last 3 years. If a tonsillectomy is required, it is best to always get a second opinion, except in an emergency such as the appearance of a phlegmon or an abscess. Phlegmon and tonsil abscess can cause respiratory distress requiring urgent intervention.
Acute articular rheumatism
the acute articular rheumatism, the AAR: This pathology occurs a few weeks after a angina caused by streptococcus. It causes damage to the joints, the heart and the membranes surrounding certain organs such as the pleura, located around the lungs. The diagnosis is confirmed by a blood test, a local sample, an X-ray, an ultrasound. The RAA represents a real emergency requiring rapid care and treatment including an antibiotic, corticosteroids and strict rest. A preventive treatment generally comprising a regular injection of penicillin is then prescribed.
Chronic tonsillitis
“Pharyngeal pain, bad breath, inflamed tonsils, cervical lymph nodes lasting at least three months despite treatment require intervention” says Dr. Patrick Aubé, general practitioner.
Removal of tonsils in adults
The operation of the tonsils in adults is not performed only if medical reasons require it.
The operation is carried out under General anaesthesia and is accompanied by antibiotic therapy. intervention (20 to 30 minutes) takes place with tracheal intubation. The intervention is carried out in passing the instruments through the mouth. Tonsillectomy can be performed on an outpatient basis in children insofar as post-tonsillectomy bleeding is discovered either before discharge or beyond the sixth day. However, not all patients can benefit from the operation on an outpatient basis.
What are the side effects of tonsil removal?
Of the sometimes hard to bear pain may occur within a few days of surgery. “In particular painful dysphagia preventing food”, says Dr. Aubé. Paracetamol treatment can reduce pain. Eating ice cream can relieve the pain. It is advisable to eat liquid for a few days. “Hospitalization may be necessary in case of dehydration in children“, underlines the general practitioner. And to specify: “You should know that tonsillectomy can cause bleeding that is quite frequent after this intervention, in generall within six hours which follow, which corresponds to the minimum time of careful monitoring of the operated person.
What are the risks after tonsil surgery?
“The risks of surgery are not negligible” estimated the High Authority of Health in a 2012 summary.
Immediate risks
- Small injuries to the tongue, lip (benign).
- Pains in the ear without gravity of the same.
- Some blood-tinged sputum.
Secondary risks
- Bleeding occurring within 8 to 15 days after the operation is rare. It must be treated quickly and any bleeding, even minimal, must be reported to the surgeon, inform the SNORL.
- Food difficulties can interfere with the taking of painkillers, or even lead to malnutrition and dehydration: this must be reported to the surgeon quickly.
- Changes in the voice due to air leakage at the level of the soft palate can be observed after healing. They may require speech therapy.
Serious and/or exceptional complications
An exceptional complication must be reported: themajor bleeding, which occurs during the operation or during the healing phase. It can impose an operation on the level of the neck to carry out hemostasis and engage the vital prognosis. The risk of death haemorrhagic origin was estimated at 1/50,000 according to the HAS.
- The child must be particularly follow-up for the first 10 days of healing.
- A liquid and cold diet is recommended the days following the operation to limit pain and the risk of bleeding.
- Fever and bleeding may occur. Consult the doctor.
- Monitor the child’s temperature and the absence of bleeding.
- It is strongly advised to fight the factors favoring chronic tonsillitis in order to avoid as much as possible the operation of the tonsils in adults.
- Keep allergens away and treat any allergies.
- Do not smoke until healing and avoid passive smoking.
- Consult in case of sinus affections or repeated nasal affections.
- It is essential to treat any angina and maintain impeccable oral hygiene.
Sources:
Medical information before performing a tonsillectomy, SNORL, 2017.
Children’s tonsillectomy. 2020 update of the SFORL & CFC recommendation.
Tonsillectomy with or without adenoidectomy in children or adolescents (under 18). Synthesis of literature data December 2012. HAS
Thanks to Dr Patrick Aubé, general practitioner.