Those who fight cancer and cancer types have been eagerly waiting for a cure to be found for years. It is a fact that cancer, which millions of people all over the world are fighting, is no longer a threat with early diagnosis and treatment.
Cancer patients, who were in the most sensitive situation with Covid-19, experienced disruption in their treatment and controls due to the uneasiness of catching the virus. Prof. from Lütfi Kırdar Training and Research Hospital. Dr. Nedim Turan answered the troubles of cancer patients during the Covid-19 process, the questions asked and the well-known misconceptions about cancer for Mynet.com.
WHAT ARE THE FACTORS THAT YOU HAVE MOST CHALLENGES IN THE TREATMENT PROCESS OF CANCER PATIENTS COMING BEFORE THE PANDEMIC? WHAT SITUATIONS HAVE YOU FACED THE MOST?
Since some patients could not come to their pre-planned control due to the pandemic, we regret that the disease got out of control, because if these patients were controlled, at least some of them could have been completely cured. However, when this group of patients, who hindered their controls, is evaluated in detail, it is understood that these patients mostly consist of patients whose treatment has been completed and who are under follow-up without medication. Others were patients who received only pill-like treatment and whose disease was in remission. Apart from these two groups, a small part of the patients could not come to their controls due to the fear of pandemic while their active treatment was continuing. In addition, the number of newly diagnosed patients decreased a little compared to the pre-pandemic period, but when we talk to our patients, we understand that our hospital was a pandemic hospital at that time and therefore some new patients went to other centers.
EARLY STAGE, EARLY DIAGNOSIS CANCER DISEASE WHAT EXACTLY MEANS? CAN YOU EXPLAIN THE SITUATION OF CAUGHT IN THE EARLY STAGE?
There is a popular expression such as “don’t be afraid of cancer, but of being late”. This expression is both very true and still an invariable rule that applies to all cancers. Because cancers do not occur overnight, they usually develop at the end of a certain period of years. This gives us a window of opportunity to recognize cancer and act accordingly. All we have to do is listen to ourselves/our body and participate in the KETEM (cancer early screening center) programs affiliated with the Ministry of Health. We can create an opportunity for early detection of cancer by participating in early screening programs for breast, cervical and digestive system cancers, which are carried out free of charge through KETEMs. In addition, by giving enough attention to our body (eg, changes in bowel habits, non-healing wounds, involuntary weight loss, increased incidence of cancer in first-degree relatives), it can be an early harbinger of a possible developing cancer. We can completely remove a cancer that is caught early from the body with a good surgery, that is, we can achieve healing by “uprooting”, so to speak. Therefore, the earlier a cancer is caught, the easier it is to treat the cancer and provide a definitive solution.
DID YOU HAVE A STATISTICALLY INCREDIBLE LIFE PATIENT WHO LIVES STATISTICALLY ABOVE AVERAGE, WHO’S DISEASE IS IN ADVANCED PHASE OR OR EXPANDED TO MANY REGIONS AND CANNOT BE SURGICAL?
Of course it did, a lot. Just as the developing technology has advanced the diagnostic and imaging methods used in our hospital, it has also taken the drugs we use in our daily practice to the next level. For example, different PET-CT subtypes can now be taken in our hospital according to the subtype of cancer. In other words, we now use different PET-CT in prostate cancer, different in neuroendocrine tumors and different in breast cancer. This enabled us to perform more precise staging, as well as strengthen our hand compared to other imaging methods, whether the medicine we give shrinks the cancer and if it does, how much it shrinks. On the other hand, our medicines have become more effective with the developing technology.
In the past, there were only chemotherapy drugs and we gave the same drugs to everyone. While some of the patients benefited from these chemotherapies, some of them could be harmed on the contrary, and since there was no better option, we would have to give chemotherapy despite its side effects. Although chemotherapies continue to be a powerful weapon in our hands today, their usage areas are decreasing day by day. Today, one out of every two patients treated in the outpatient clinic now uses molecular smart drugs or immunotherapy. With the immunotherapy agents and molecular-targeted drugs that we are increasingly using, the side effects we encounter have both decreased and the lifespan of our patients has been extended as the rate of disease control has increased. Even in patients with all-pervasive stage-IV cancer, we even have patients whom we consider to be cured, since the duration of disease control in some cancer types with immunotherapy exceeds five years. For this reason, we believe that with the introduction of immunotherapy into our lives, disease control rates and even cure rates will increase. By the way, I would like to explain the difference between immunotherapy and molecular smart medicine in one sentence as it sometimes creates confusion in the society.
Molecular smart drugs; It neutralizes the cancerous cell by targeting a special molecule formed in the cancerous cell at the end of a pathological process. Immunotherapy, on the other hand, does not directly target cancerous cells, instead, it directs the person’s own healthy immune cells to the cancerous area, allowing the immune cells to recognize and destroy the cancerous cell. In the meantime, molecular smart drugs and immunotherapy have been applied in our hospital’s medical oncology outpatient clinic for a long time.
IN GENERAL, ONCOLOGISTS DO NOT MAKE SOLID RULES ABOUT THE NUTRITION OF CANCER PATIENTS. IS THIS TRUE? IF YOU EVALUATE CANCER PATIENTS IN A GENERAL FRAMEWORK, HOW TO NUTRITION? WHAT TO STAY AWAY FROM COMPLETELY?
A balanced diet is very important in cancer patients as well as in healthy people. We know that a number of dietary factors may be effective in the development of some cancers, for example, the effects of nitros-amine containing foods or high-salt diet in the development of gastric cancer have been shown in studies. However, randomized studies have not shown that any dietary changes affect survival after cancer has developed. In fact, although this issue (the effect of diet change on survival in patients with cancer) has been questioned in many studies and some recommendations have been made, different results, and sometimes even the opposite, have emerged in each study.
In addition, the overwhelming majority of studies are not randomized and many have methodological problems. For this reason, there is currently no specific dietary recommendation on which a consensus has been reached. Our only fear about the diet in cancer patients is that microorganisms in the vegetables and fruits that are not sufficiently washed while receiving chemotherapy can cause infection, because chemotherapy suppresses the immune system and makes the patient vulnerable to infections. In short, we do not recommend dietary restrictions as long as it is hygienic. The ones that should be avoided completely are herbal agents that are claimed to be “healing”, alcohol and cigarettes.

THE PATIENTS FREQUENTLY CONSIDER THAT THERE IS AN EFFECTIVE TREATMENT FOR CANCER, BUT IT HAS NOT YET BEEN ANNOUNCED. DO YOU BELIEVE THERE IS JUSTICE IN THIS FORECAST?
I do not want to be anyone’s lawyer in this matter, and I do not want to leave anyone under suspicion. I can only say that, if an institution whose main purpose is commercial, had such a drug, why wouldn’t it want to earn more? That’s why I see this issue more as a magazine issue.
WHY IS SELECTION OF ONCOLOGIST SO IMPORTANT FOR A PATIENT? WHAT IS THE EFFECTIVE ROLE OF AN ONCOLOGIST IN THE TREATMENT OF CANCER PATIENT?
In my opinion, it would be more appropriate to call it a medical (medical) oncologist instead of an “oncologist”, because such confusions in terms can sometimes lead to problems of contact while patients seek solutions to their problems. For this reason, it is necessary to summarize briefly what trainings the branches dealing with oncology have received and which problems can be solved. Thus, patients will better understand which branch they should deal with while seeking solutions to their problems.
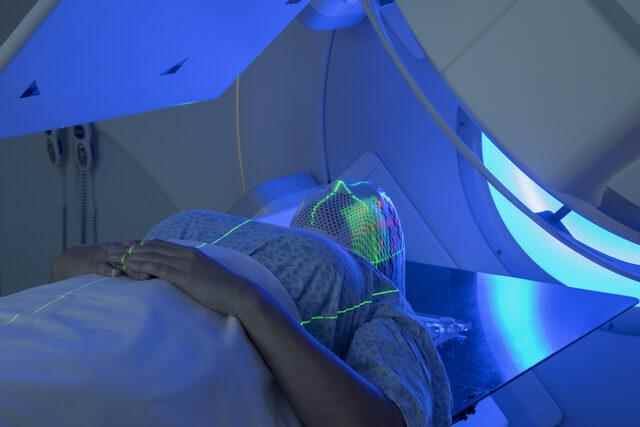
For example, a medical oncologist completes 4 years of internal medicine residency training after medical school and receives the title of medical oncologist after completing an additional 3 years of medical oncology training, while a radiation oncologist receives the title of radiation oncology specialist with 5 years of radiation oncology training immediately after graduating from medical school. . During this training, medical oncologists learn how to treat which cancer with which drugs (chemotherapy, molecular agents and immunotherapy), how to prevent possible side effects of cancer drugs on internal organs and how to fight in case of organ damage. On the other hand, while the radiation oncologist learns the effects and side effects of radiation on the body during his residency training, he learns how to use radiotherapy in which cancer, in which dose and in what way, and how to manage possible side effects. The specialty training of surgical oncologists, on the other hand, is similar to the training of medical oncologists and learns how to operate on cancers of organs related to their own branch and how to manage possible complications related to surgery. It should not be forgotten that apart from the branches I mentioned above, radiology, nuclear medicine, pathology and other branches also play an important role in the management of cancer patients.
Returning to your question after briefly summarizing the areas of specialization dealing with cancer, I can only make a personal comment on behalf of medical oncology. From the point of view of the cancer patient, I think that the knowledge of the physician, the ability to provide information in a language that the patient can understand, the ability to empathize and to give morale even in the worst scenario, are highly valued by the patients. I also observe very often that most of the patients are attached to their first medical oncologist with a sense of trust and do not want to leave the same doctor for life.
YOU HAVE CARE WITH NUMEROUS PATIENTS TODAY… DO YOU HAVE A DIFFERENT ONCOLOGICAL CASE YOU CAN SHARE WITH US?
With pleasure… I can never forget the moment when an associate professor of pulmonology at the hospital I worked for was diagnosed with blood cancer during my internal medicine residency training. While examining the blood smears of the patients in the microscope room with our own teacher, when our associate professor, who had been resting at home for a week with the diagnosis of cold, entered the microscope room and said jokingly, “How long do I have left, my teacher,” because he was not aware of the seriousness of the incident, everyone inside turned into ice. I still remember the shock on the face of our hematology teacher and her struggle to explain the seriousness of the event, and I think I will never forget it. I hope and wish that no physician friend will experience that elusive feeling we experience. Thank you.
