Thanks to anti-bacterial treatments, life expectancy has increased by at least ten years. But after a century of use of these treatments, sometimes in an abusive way, their effectiveness is threatened: certain bacteria can adapt and resist the treatments. According to the World Health Organization (WHO), antibiotic resistance is one of the most serious threats to global health today.
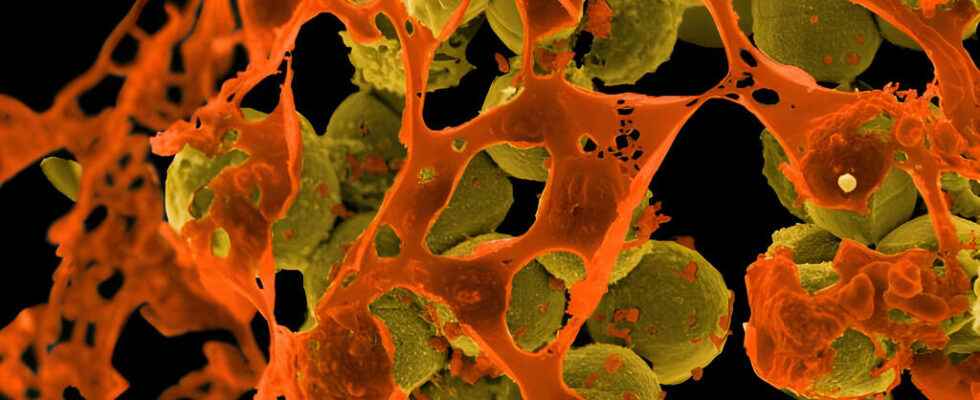
To fight against highly resistant bacteria, such as Staphylococcus aureus, it is necessary to develop a new generation of antibiotics.
The discovery of penicillin, in 1928 by Alexander Fleming, marked the birth of antibiotic treatments as well as therapeutic medicine. Millions of lives have been saved each year since the advent of antibiotics. It took several years of research, after Fleming’s discovery, for penicillin to be mass produced and used. Undoubtedly, the first large-scale use took place during the Second World War, allowing to treat the wounded or diseases such as tuberculosis and typhoid.
The mechanism of an antibacterial molecule is quite simple: the drug stops bacteria from growing and multiplying, then eventually kills them completely. The other side of the coin: bacteria can adapt and even resist treatment with antibiotics.
The resistance mechanism
The WHO, in the first report on antimicrobial resistance in 2014, sounded the alarm. ” This grave threat is no longer a prediction, but a reality with every region of the world moving into a post-antibiotic era, where common infections or even minor injuries could kill again. “, worries the world organization which considers this problem as an emergency.
Indeed, around 1.2 million deaths were recorded in 2019. Deaths directly linked to antibiotic-resistant infections, underlines a report published in January 2022 by the scientific journal The Lancet. In addition, the study shows that 26% of infections have resisted the treatments that are generally prescribed, but that in 2050, this proportion of resistant bacteria will almost double. In short, infections are already more difficult to treat in humans and animals, because the number of bacteria resistant to certain antibiotics continues to increase. But bacteria can also develop resistance to several families of antibacterial drugs: we then speak of “super-bacteria” or “multi-resistant bacteria” (the Anglo-Saxon name great bug is also often used).
Above all, it is the useless use of an antibiotic that is singled out. The specialists are formal: taking an antibacterial drug will above all contribute to increasing the genetic power of bacteria to adapt to resist in the event of a bacterial infection. And when taking these drugs is useless, when it comes to treating viral infections or the flu, the bacteria then learn even better to defend themselves against the molecules supposed to eliminate them. Taking an antibiotic for no real reason increases the risk of a future infection that is difficult or even impossible to treat.
Worrying consequences
According to the National Institute of Public Health of Quebec, more and more patients must receive doses composed of several types of antibiotics that are often more harmful to patients. The same source points out that gonorrhea is among the most difficult bacterial infections to treat today. The bacterium that causes the sexually transmitted infection has become highly resistant to antimicrobial treatments, with the risk of becoming uncontrollable in years to come. Already in 2019, the WHO warned that antimicrobial resistance is among the ten greatest public health threats to all of humanity. And this is not without reason, because the bacteria responsible for cholera, different kinds of pneumonia, legionellosis, meningitis are also part of the pathogenic species which have incredible capacities to adapt their genetic code to become more resistant.
The development of super-bacteria is increasing almost everywhere in the world, but their emergence is especially visible in developing countries. With an inefficient healthcare system lacking means of prevention, the sale of antibiotics is free and without prescription. Their uncontrolled use greatly contributes to the increase in bacterial resistance.
In parallel, intensive farming and animal husbandry are largely responsible for the amplification of the phenomenon. In the Americas, it is common for farmers to give their animals high doses of antibiotics, even as a preventive measure. In France and since 1999, the National Agency for Food, Environmental and Occupational Health and Safety (ANSES) has set up monitoring of the sale of veterinary medicinal products. According to this agency, from 2011 to 2020, the overall exposure of animals to antibiotics has decreased by approximately 45% compared to the previous decade.
What solutions?
Faced with this global problem of resistant super-bacteria, the scientific community began looking for a solution to avoid a regression of world medicine more than a century back. For this, the development of new antibiotics is absolutely urgent. The objective is to find a treatment that would be as selective as possible, that is to say, to narrowly target the bacteria and only those which are at the origin of the infections. In this way, it would be possible to limit the speed of resistance development. However, researchers in the pharmaceutical industries are confronted with the problems of funding their work, because antibiotic treatments are not sold at high prices and, consequently, do not bring in enough to allow adequate funding for research. Despite the lack of funds, a few new molecules have been available for about five years, such as ceftolozane, whose abilities have proved convincing against bacteria that have become multi-resistant.
In addition, one of the solutions studied is that of phage therapy : the virus that targets and kills bacteria. A technique which, still, is not available on a large scale.
Despite findings by the WHO that the misuse of antimicrobials is an “invisible epidemic” that could be deadlier in the long term than Covid 19, claiming more than 10 million deaths a year, there are reasons to hope for a less bleak future.
Indeed, in May 2015, several international organizations such as the WHO, the Food and Agriculture Organization of the United Nations (FAO) and the World Organization for Animal Health (OIE) adopted a common plan to on a planetary scale to combat the proliferation of bacterial resistance. This plan emphasizes the need to raise awareness among the public and health personnel, to strengthen surveillance, research and hygiene measures, and to optimize the use of antibiotics.
► To read also:
Antibiotic resistance kills more people than AIDS or malaria
Antibiotic resistance responsible for 13,000 deaths per year
A lot of hope after the discovery of a new antibiotic
The NDM-1 bacterium, resistant to almost all antibiotics
► To listen:
Antibiotic resistance
Antibiotic resistance: what are the risks?
In the Central African Republic, the fight against antibiotic resistance is accelerating
The proper use of antibiotics