Published on
Updated
Reading 2 min.
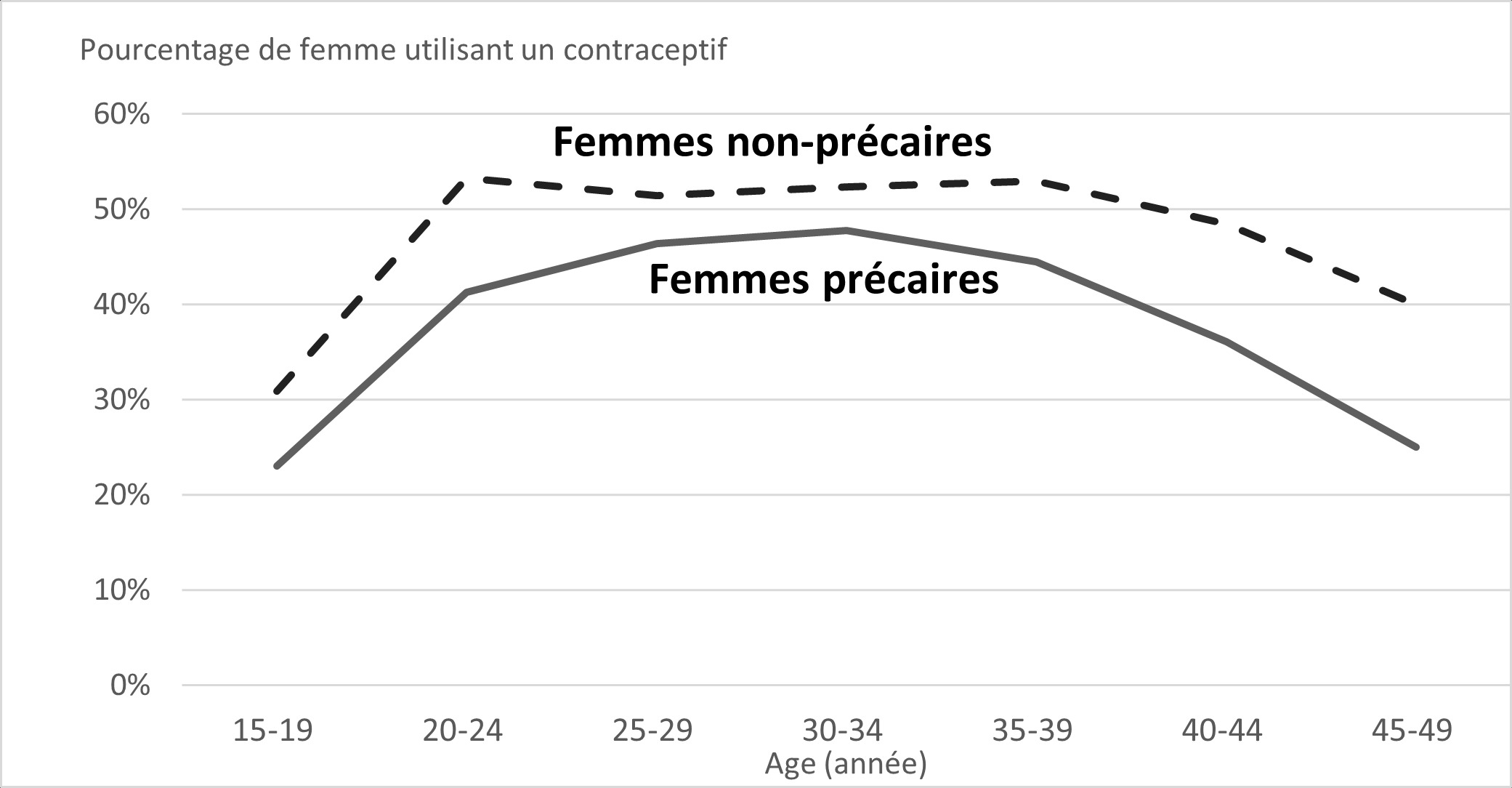
Women with lower incomes use reimbursed contraceptives less than others, at all ages of their reproductive life. The choice of contraceptives is also different.
Women with modest incomes use reimbursed contraceptives less
Only 36% of low-income women use a reimbursed contraceptive, compared to 46% of women with higher incomes, indicates this study by the National Institute of Demographic Studies (INED), carried out in collaboration with the National Institute of Health and medical research (Inserm). “This disparity persists regardless of the age of women“, specifies an INED summary.
Health Insurance reimburses certain contraceptive pills, hormonal contraceptive implants, injectable progestins, intrauterine devices (IUDs) or IUDs and diaphragms.
The INED study shows that “the removal of a financial barrier, through reimbursement, does not guarantee the absence of other barriers which could hinder access to contraception for low-income women“, notes the study.
These women could, for example, meet “difficulties in accessing contraceptive prescribers” or administrative difficulties in maintaining their social security coverage leading women to turn to non-reimbursed contraceptives so as not to have to consult a doctor or midwife to obtain a contraceptive.
Different choices of contraceptives depending on income
In detail, low-income women aged 20 to 24 use oral contraceptives less (23% versus 38%) and more implants than those with average or high incomes (8% versus 4%). At ages 45 to 49, low-income women use a hormonal intrauterine device (IUD) less frequently (6% versus 14%).
These different uses are not fully explained, but the authors hypothesize that low-income women and young people are often targeted in public health contraceptive programs due to a higher risk of unwanted pregnancies. Therefore, health professionals could encourage the use of more effective contraceptives, such as the implant. Access to a gynecologist could also be particularly complicated for low-income women and explain the low use of hormonal IUDs.
“A thorough understanding of the barriers to contraceptive use is crucial to enable women to make informed choices about the spacing and timing of their pregnancies.“, underlines INED.
This study was carried out on health insurance data from 14.8 million women, aged 15 to 49, living in France in 2019. Among them, 11% lived below the monetary poverty line, or around 1,100 euros for a single person.
