Optic neuritis corresponds to a sudden and significant suffering of the optic nerve with, always, an inflammatory cause. Singer Hélène Ségara has had it since 2013. Cause, autoimmune disease, cure: all you need to know.
Optic neuritis is a inflammatory damage to the optic nerve which transmits visual information to the brain. This eye disease can lead to a sudden partial or complete loss of vision. Among the causes, an autoimmune disease such as multiple sclerosis. There a singer Helene Segara suffers from optic neuritis since 2013. In February 2022, she had to resign herself to canceling her concerts “after several months of heavy treatment, in the greatest secrecy” she then explained on her account instagram. Causes, symptoms, treatments, optic neuritis cure with doctors Chafik Keilani and Edouard Augstburger, ophthalmic surgeons at the CHNO des Quinze-Vingts.
What is optic neuritis?
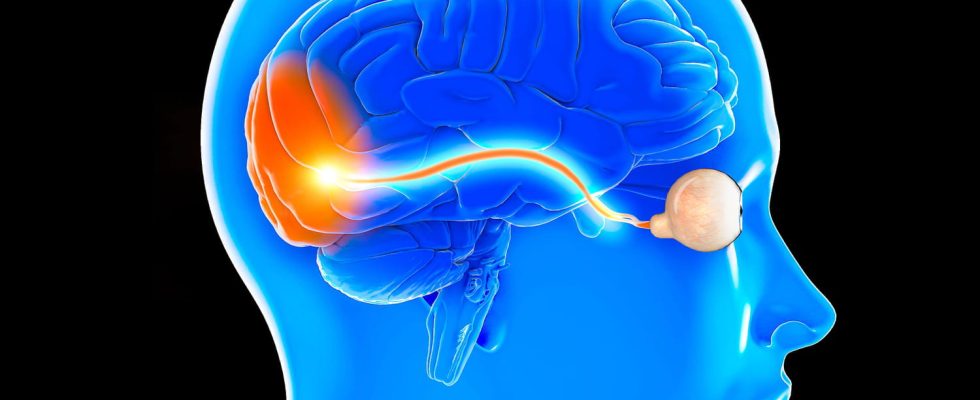
Optic neuritis is a type of optic neuropathy characterized by acute suffering of the optic nerve of inflammatory origin. The optic nerve is a cranial nerve that transmits visual information from the eyeballs to the brain. optic neuritis can cause sudden partial or complete loss of vision. Depending on the location, we distinguish:
- THE papillitis which reach the anterior part of the optic nerve.
- THE retrobulbar optic neuritis where the nerve damage is behind the eyeball.
What is retrobulbar optic neuritis?
“The term retrobulbar optic neuritis is often used to clarify that theinflammatory damage to the optic nerve located behind the eyeballas opposed to papillitis, in which the inflammation affects only the initial portion of the optic nerve at the level of the papilla, in the eyeball“says Dr. Augstburger. The most common cause of retrobulbar optic neuritis is multiple sclerosis. But there are also other causes like infectious causes (syphilis, Lyme disease,
herpes, …), medication or secondary to vasculitis.
What is ethyl optic neuritis?
Ethyl optic neuritis is a dysfunction along the optic nerve in association with chronic alcohol consumption. The toxic role of alcohol is not clearly established, but it leads to nutrient deficiencies especially of B vitamins responsible for this malfunction.
What is bilateral optic neuritis?
Bilateral optic neuritis from optic neuropathy is characterized by acute pain in both optic nerves (right and left). It is rare and the causes mentioned above must be sought, in addition to brain damage.
What are the causes of optic neuritis?
There are several causes of inflammation of the optic nerve:
- THE autoimmune diseases of which the multiple sclerosis which is a demyelinating condition of the central nervous system.
- THE Infectious diseases such as bacterial infections including tuberculosis, syphilis or even viral infections including HIV (human immunodeficiency virus).
- THE metastases affecting the optic nerve.
- I’absorption of toxic substances such as lead, tobacco, certain drugs including quinine.
- THE vitamin deficiencies including vitamin B. These deficiencies are often present in alcoholic people.
- Idiopathic i.e. unknown cause.
“The most common cause of retrobulbar optic neuritis is multiple sclerosis. For this reason, optic neuritis most often occurs in adults between the ages of 20 and 40. She touches preferentially Caucasian populations and the female gender“says the ophthalmologist.
Is multiple sclerosis a cause of optic neuritis?
Yes, she is one of them. It is the most common cause of retrobulbar optic neuritis. “For this cause, optic neuritis most often occurs in adults between the ages of 20 and 40. She touches preferentially Caucasian populations and the female gender“says the ophthalmologist. In case of autoimmune cause related to multiple sclerosisA corticosteroid treatment administered intravenously may be prescribed to speed healing.
Initially, partial or complete loss of vision on the side where the neuritis occurs.
What are the symptoms of optic neuritis?
“The onset of optic neuritis is often acute and there is a partial or complete loss of vision on the side where the neuritis occurs, points out Dr. Augstburger. It can also occur visual blurring. Loss of vision can sometimes be accompanied by headaches and retroocular pain triggered by movements of the affected eye. Faced with a loss of vision or retro-ocular pain triggered by eye movements, an ophthalmologist should be consulted.
The diagnosis is made by an ophthalmologist and/or a neurologist. First, a clinical examination is performed. The ophthalmologist quantifies vision. Then he does a pupil test. Finally, he makes a fundus examination to examine the retina and the papilla which is the head of the optic nerve. The fundus may initially be normal or show edema. Secondarily, the papilla becomes discolored, which testifies to optic atrophy. The ophthalmologist can also complete the examination with a visual field which evaluates the part of the space that an eye can perceive around the point it is fixing. Confirmation of the diagnosis is made by magnetic resonance imaging (MRI) of the brain and optic nerves. It can highlight an enlarged optic nerve. In other cases, this finding may be associated with the presence of brain lesions compatible with multiple sclerosis. The diagnostic confirmation can also be done using the method of visual evoked potentials which aims to measure the electrical activity of the nerve pathways of vision.
“Most cases resolve favorably, with vision returning within 2 to 3 months.”
What are the treatments for optic neuritis?
The treatment of optic neuritis essentially consists of treating its cause:
- In case of infection, anti-infective treatment is prescribed.
- In case of vitamin deficiency, vitamin supplementation is carried out. If a toxic cause exists, the exposure by this toxic agent must be stopped.
- Finally, in the event of an autoimmune cause related to multiple sclerosisA corticosteroid treatment administered intravenously may be prescribed to speed healing.
Can optic neuritis be cured?
“The prognosis depends on the underlying cause. Most cases resolve favorably, with return of vision within 2 to 3 months that follow, reassures Dr. Augstburger. Appropriate management allows remission of inflammation of the optic nerve. The pain disappears and the vision improves. Sometimes visual recovery is imperfect and inflammation continues“. In this case, anti-inflammatory treatment with corticosteroids can be prescribed. There is no specific prevention for optic neuritis. However, it is recommended toavoid alcohol and tobacco poisoning and to regularly consult an ophthalmologist because recurrences may exist.
What is the evolution of an optic neuritis?
The course depends on the cause. Generally, symptoms of optic neuritis such as pain or blurred vision go away. For a small minority of cases, visual function tends to deteriorate. Finally, for some patients, a recurrence of optic neuritis in either eye may exist. This is the case, for example, of patients with multiple sclerosis.
Thanks to Doctors Chafik Keilani and Edouard Augstburger, ophthalmic surgeons at the CHNO des Quinze-Vingts in Paris. Comments collected in 2020.