The World Health Organization (WHO) announced that the number of monkeypox cases reported to them in the current epidemic has exceeded 1,000, except in countries where it is more common in Africa.
Tedros Adhanom Ghebreyesus, WHO Director-General, said that the risk of monkeypox settling in these non-endemic countries is real, but preventable at this stage.
In the current epidemic that started in May, cases were reported from 29 countries outside of Africa, but no deaths have been reported yet.
At a press briefing in Geneva, Ghebreyesus said there were also more than 1,400 suspected cases of monkeypox in Africa this year, with 66 deaths.
“It is an unfortunate reflection of the world we live in that the international community is only now paying attention to monkeypox because it originated in high-income countries,” said the WHO Director.
He said that the epidemic showed signs of transmission in the community in some countries. WHO recommends that people with monkeypox be isolated at home.
Healthcare professionals treating patients are advised to wear masks.
The WHO added that although cases have also been reported in women, most cases still occur predominantly among men who have sex with men.
In its previous statement dated May 21, WHO stated that the symptoms lasted between 2-4 weeks, and the mortality rate was between 3-6 percent.
Hans Kluge, WHO Europe Director, said: “As summer approaches, I am worried that the spread will accelerate due to big gatherings, festivals and parties.”
He also shared the most frequently asked questions and answers about monkeypox from the WHO website.
Some of them are as follows:
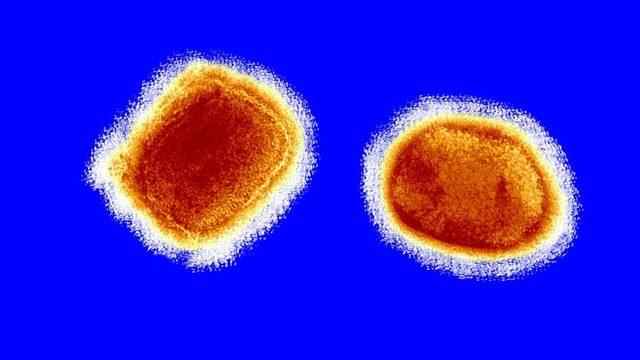
There is a genetic similarity between the smallpox virus, which was wiped off the face of the earth in 1980 after the global vaccination activity, and monkeypox.
Therefore, people who are vaccinated against smallpox can have some protection against monkeypox.
On the other hand, the disappearance of the virus from the ground more than 40 years ago and then the cessation of vaccination activities makes the young population more vulnerable to this virus.
Animals carrying this virus, which are frequently found in Central and West Africa, live in the tropical rainforests of those regions.
It is thought to have spread to other regions through people traveling from these regions and animals sold.
Symptoms include fever, intense headache, muscle aches, back pain, fatigue, lymph node swelling, skin rash and lesion.
The rash usually begins 1-3 days after the fever.
Lesions can be flat or swollen, fill with a clear or yellowish fluid, and then often crack, dry and fall off.
The number of lesions in the body can vary from a few to thousands.
The rash is usually concentrated on the face, palms and feet, but is less common on the trunk.
They also appear in the mouth, genitals, and eyes.
These symptoms usually go away on their own after 2-4 weeks.
However, when symptoms occur, it is recommended to consult a doctor rather than wait for them to go away on their own.
Those who have close contact with those who have had monkeypox are also advised to notify the health units.
In most cases, the symptoms go away on their own, but the virus can be fatal for some people.
This virus poses a greater threat to newborn babies and people with weakened immune systems.
In severe cases, skin infections, pneumonia and eye infections that can progress to blindness can be seen.
In African countries where cases are most common, the mortality rate varies between 3 and 6 percent.
However, due to the limited virus detection systems in these countries, there is a high probability that mild cases will not be detected.
Therefore, the actual death rate may be lower than that.
Animals carrying the virus can transmit it to humans through physical contact. These animals include rodents and primates.
In order to reduce the risk, it is recommended not to come into unprotected contact with wild animals, especially to stay away from sick animals or dead animals.
People who carry the virus are contagious when they show symptoms. This usually happens 2-4 weeks after exposure to the virus.
Especially rash areas, body fluids and wounds can be contagious.
Clothes, towels, bed linen and cutlery used by people carrying the virus can also transmit the virus.
Since lesions and wounds in the mouth are also contagious, there is a possibility of transmission through saliva.
Therefore, those who are in close contact with people with monkeypox virus, especially those living in the same household, sex partners and healthcare workers are at higher risk.
The virus can also pass from the placenta to the baby during pregnancy.
It is unclear whether patients who do not show symptoms are contagious.
Young people, as well as those in close contact with those carrying the virus, are thought to be at greater risk.
The reason for this is that the elderly have some immunity to monkeypox due to smallpox vaccination.
Babies, children and people with weakened immune systems are also at risk.
The most effective way of protection is to reduce physical contact with people suspected of carrying the virus.
It is recommended that healthcare workers and those living with those carrying the virus do not come into direct contact with the lesions and wear a mask, cover their wounds, isolate themselves and wear a mask.
Wearing disposable gloves when physical contact is necessary reduces the risk of contamination.
People living in the same household need to regularly clean surfaces, clothes and utensils.
Monkeypox virus shows more symptoms in children and newborn babies.
If you think you have been exposed to the virus, you should apply to health institutions and isolate yourself as much as possible during this process.
After the application, health institutions can reveal whether you are positive as a result of their tests.
Vaccines developed against smallpox also provide partial protection against monkeypox.
A vaccine called MVA-BN, produced under the brands Imvamune, Imvanex, and Jynneos, approved in 2019 is also effective against monkeypox, but is still in limited production.
Disease symptoms usually go away on their own. It is also recommended to wait for the rash and itching to dry on their own, if possible, and to keep it moist if not.
It is also important not to come into contact with wounds in the eyes and mouth.
The antiviral drug tecovirimat (also known as TPOXX) developed against smallpox was also approved for use against monkeypox in January 2022.
Monkey pox has been seen in 11 African countries since 1970. These are Benin, Cameroon, Central African Republic, Congo, Democratic Congo, Gabon, Ivory Coast, Liberia, Nigeria, Serra Leone and South Sudan.
Usually, the virus can be seen in other countries due to people traveling from these countries.
One of the epidemics occurred due to animals imported from these countries.
The cases seen in Europe, America and Australia in May 2022 were an extraordinary spread in the history of the virus. It was noticed that many cases were not related to African countries.
The World Health Organization continues to investigate the causes of this spread and to support countries that have seen the virus.
Monkeypox is not considered a highly contagious virus. This is because it requires physical contact to be transmitted.
The World Health Organization, which has long evaluated this virus in the high priority virus category, contacted the countries where the virus was seen to prevent the spread of the virus.
Monkeypox virus is transmitted by physical contact, and this includes sexual intercourse.
It is not yet known whether the virus is transmitted through vaginal fluids and semen, but skin contact during sexual intercourse may be sufficient to transmit the virus.
Symptoms on the skin can resemble those of other viruses, such as sexually transmitted syphilis and herpes.
This may explain why the virus is mostly seen in men presenting to sexual health clinics.
But the risk isn’t just limited to sexually active people or men who have sex with men.
In cases in European countries, men who had intercourse with men were detected among those infected with the virus. These cases were diagnosed when they presented to sexual health clinics.
The reason why more cases are heard in this group may also be due to the fact that this group is more sensitive about sexual health.
The virus got this name because it was first detected in a monkey colony used in scientific research in 1958.
The first virus in humans was seen in 1970.