A nurse practitioner in Perth County says she’s feeling “hopeful” this week as the Ford government begins rolling out a plan to address serious staffing shortages in Ontario’s health-care system.
Wendy Dunn splits her time between two area long-term care homes – one in Stratford and one in Milverton. She’s witnessing first hand the health-care crunch that’s chasing away workers and causing sporadic emergency room closures in rural Southwestern Ontario.
“(It’s) been very difficult,” Dunn said this week. “The ones that are still working are working more and not always being given vacation and time off. In long-term care, it’s not like we can shut some beds down. The jobs are still there and need to be done.”
In many cases, hiring agencies have been trying to fill the gap in long-term care. Those hands are appreciated, Dunn said, “but it’s not the answer.”
“You always have this kind of revolving nature which … is really stressful on staff that are permanent because you’re always training,” she added. “We’ve got to figure out how to employ and keep people here locally.”
Some help might finally be on the way.
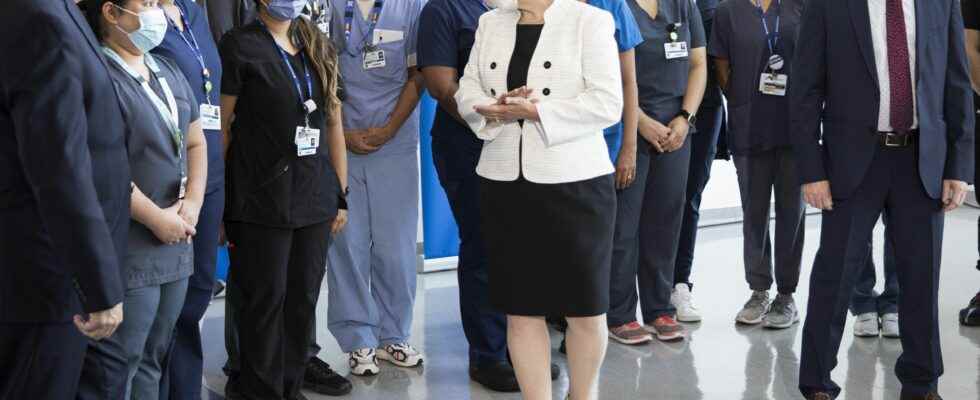
Health Minister Sylvia Jones has told the province’s nursing college to go ahead with regulatory changes that could get thousands of internationally trained nurses into practice more quickly.
The College of Nurses of Ontario – a regulator that oversees 192,000 registered nurses, registered practical nurses and nurse practitioners – has said the changes could help the 5,970 active international applicants living in Ontario and make it easier for retired nurses to re-certify.
Long-term care homes are familiar with internationally trained nurses, Dunn said. In the past, many of them have practiced as personal support workers in that sector while gaining the experience and education needed to move on.
“I don’t know where we would be if it wasn’t for that group of very willing bodies to come in and assist and be part of our teams,” Dunn said.
The idea – part of the Ford government’s five-point plan to stabilize Ontario’s teetering health system – also has the support of the Registered Nurses Association of Ontario.
Internationally trained nurses “have been waiting far too long to get registered to practice and help their fellow colleagues,” RNAO president Dr. Claudette Holloway said after Jones and Long-Term Care Minister Paul Calandra unveiled the latest phase of the government’s Plan to Stay Open last month. “Ontarians desperately need them on the front lines.”
Besides further expanding Ontario’s health workforce by hiring up to 6,000 additional health-care workers, the government’s plan also contains measures aimed at preserving hospital capacity, reducing surgical waitlists, and easing pressure on emergency departments.
The plan has been welcomed by health-care advocates, including the RNAO, who desperately want to see more nurses plugged into the system.
“We are glad the government now recognizes the magnitude of the nursing crisis and the central role of stakeholders like RNAO to find solutions so our health system can meet the care needs of Ontarians,” Holloway said. “Without nurses, you cannot run an effective functioning system, and without registered nurses and nurse practitioners, you cannot run emergency departments, transplant units, critical care or other high-intensity services – full stop.”
Parts of the plan, however, have also drawn how.
The plan doesn’t include repealing Bill 124, the controversial legislation capping compensation for public-sector workers, including nurses, at one per cent.
Some hospital officials have also raised concerns about increasing surgeries at private clinics covered by OHIP.
Andrew Williams, the chief executive of the Huron Perth Healthcare Alliance, is among them.
“If there’s going to be additional resources invested, we should be investing those dollars into existing organizations like ours to allow us to increase surgical volumes, not to create a parallel system,” he said. “We don’t have enough staff to support both.”
Adding workers to the province’s health-care system, especially in rural areas where it can be more difficult to recruit, should be the focus, Williams added.
“We’re going to do everything in our power to support the short-term plans to be responsible and provide great access to local care but we need some longer-term plans that help us set the system up to succeed,” he said. “We’re going to work closely with the government and we’re very committed to strengthening our local health system, but we do know to truly achieve that … we have to start to really rethink our system as a whole.”
In the meantime, Dunn said she’s pleased to hear the government plans to bring 225 additional nurse practitioners into Ontario’s long-term care homes.
“At least it’s a start,” she said. “It’s a first step to coming out of this.”
-With files from Postmedia News and the Canadian Press