Headaches affect approximately 66.6 %of people around the world and are often seen with psychiatric comorbidities. Previous research associated migraine with higher suicide thoughts and behaviors, but all headache Data on this relationship are limited. This gap shows that suicide tendency should be more investigated in patients with headache disorders.
Published in Jama Neurology magazine “headaches diagnosed in people Suicide Initiative and suicide risk “in the study, the first time between 1995-2020 headache diagnosed as headache 15 years and old Citizens, registered headaches with people who do not diagnose 5 to 5 to 1.
119,486 people who were diagnosed with headaches in the cohort and 597,430 paired controls were included in the diagnosis of headache. International diseases and relevant health problems statistical classification, diagnostic codes from the tenth revision caught migraine, tension -type headache, post -traumatic headache and trigeminal autonomic sefalgia.
Risk difference emerged

While the absolute risk of 15 years of attempting suicide of individuals diagnosed with headaches was 0.78 %, this risk was 0.33 %in the paired control group, which showed a 0.45 %risk difference.
Completed suicide reached a 15 -year absolute risk of 0.21 %compared to 0.15 %in controls and provided a 0.06 %risk difference. Adjustable hazard rates, headache disorder diagnosed as 2.04 for initiatives and 1.40 for deaths were significantly higher, and stronger relationships in post -trauma headache and trigeminal autonomic cephalgies (TACs) were seen.
The risk of illness is also more
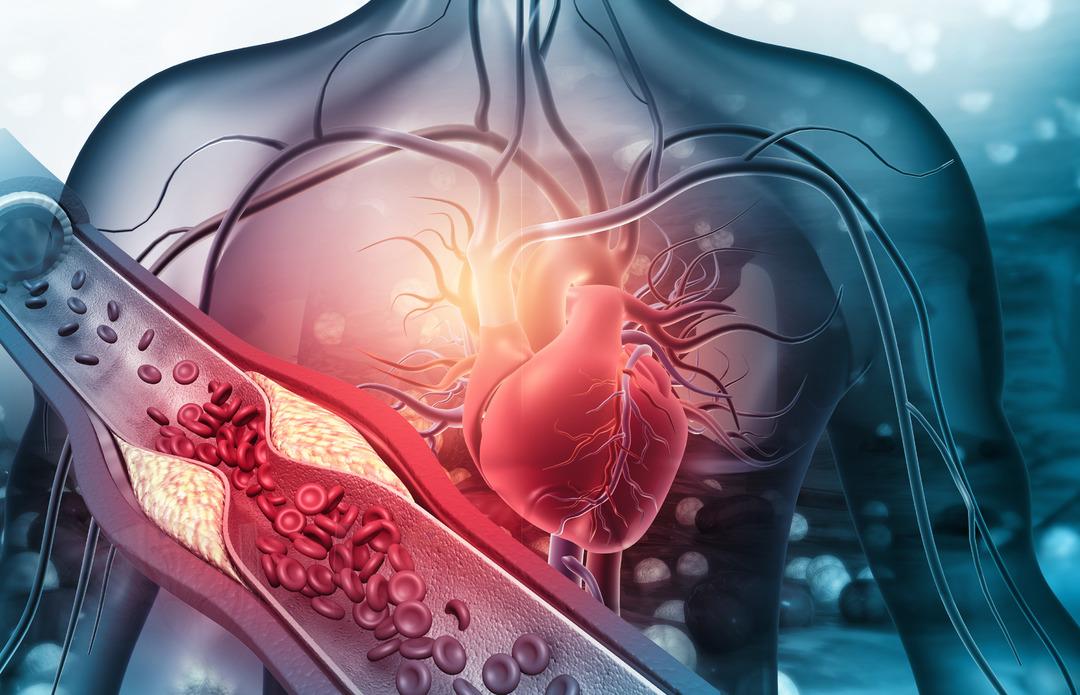
Cancer, cardiovascular disease, chronic obstructive pulmonary disease, stroke, head trauma, mood disorders, substance use disorders, and others, including cancer, had higher proportions in people with headache.
Controlling these basic diagnoses still found a permanent relationship between headaches and increasing risk of suicide. This relationship was smaller between individuals with mood or substance use disorders, but continued to exist. Increasing risk continued independently of gender, age, income or education history.
The findings from the study suggest that early assessment and focused behavioral health interventions may be important especially for people who are diagnosed with headaches.
