Published on
updated on
Reading 3 min.
In China, scientists have achieved a surgical feat: transplanting stem cells into a type 1 diabetic patient, to enable her to produce her own insulin. The young woman, aged 25, has been able to do without her injections for more than a year now.
A 25-year-old Chinese woman with type 1 diabetes underwent a transplant of cells derived from her own adipose tissue to treat her pathology. This experience is a success since for more than a year now, the patient has no longer needed to inject insulin, which is essential for controlling her blood sugar levels.
“I can eat sugar now”
Published in the journal cellon September 25, these results were obtained by Shusen Wang and his colleagues at Nankai University. To achieve this feat, the authors of this work were interested in stem cells. These immature cells can be reprogrammed to perform the functions of any cell in our body.
To obtain these “reprogrammable cells”, Chinese scientists took fat cells from three patients. All cells were returned to a pluripotent state and then programmed to produce insulin. The researchers modified the standard approach by exposing cells to certain molecules rather than introducing proteins. The patient treatment process was staggered over time so that the results from the first patient could be applied to the second, then the third.
For this young woman, these cells were injected in June 2023 into the muscles of the patient’s abdomen. The intervention lasted less than half an hour. “By placing them in the abdomen, we could monitor the cells using magnetic resonance imaging and potentially remove them if necessary” the scientists said. And two and a half months later, his body started producing insulin.
The young woman no longer needs to inject insulin
It is now under observation and for the time being, the transplanted cells have maintained a high level of production. The young woman can therefore do without exogenous insulin. She regained stable control of her blood glucose level, which remained at a normal level for more than 96% of the day.
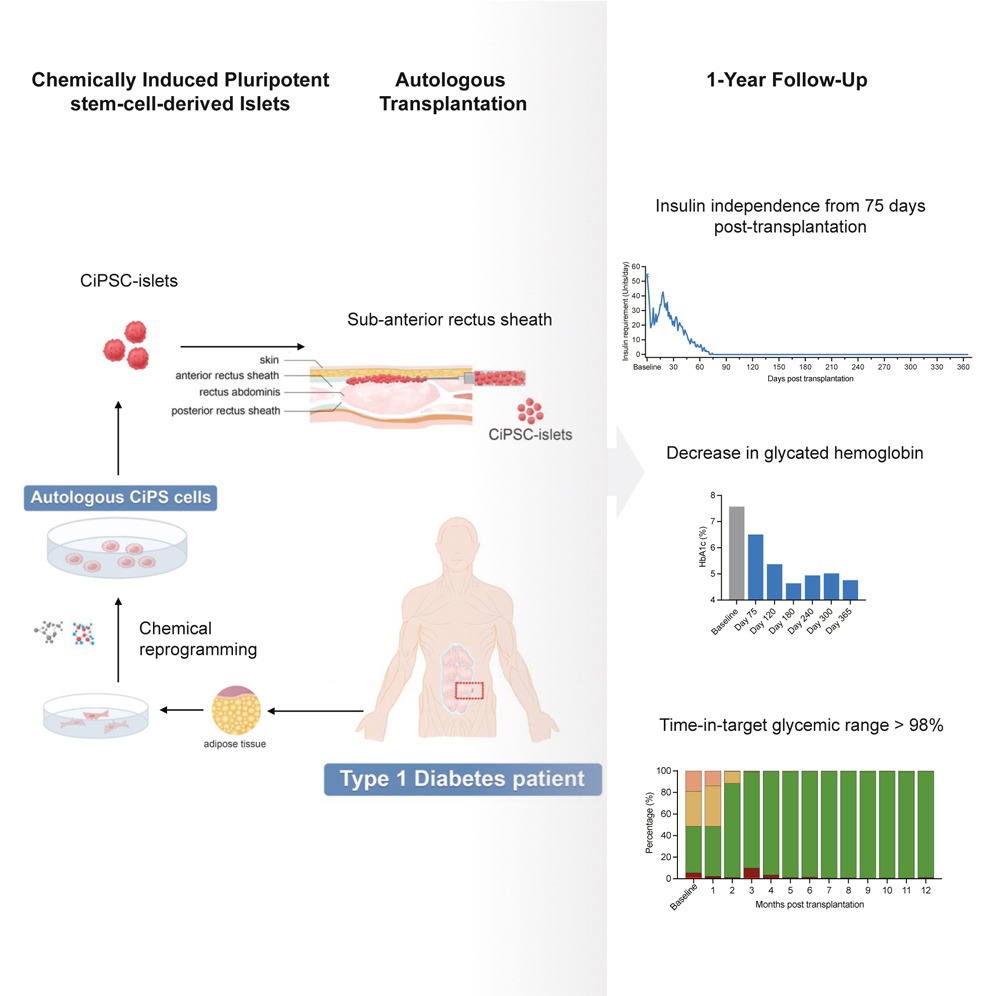
“Its target glycemic range increased from an initial value of 43.18% to 96.21% at the fourth month after transplantation, accompanied by a decrease inglycated hemoglobinan indicator of long-term systemic glucose levels at a non-diabetic level” we can read in the study. A rebirth for the one who “previously needed large amounts of insulin“. The researchers want to confirm the result of the experiment by following up this patient at 5 years.
What is type 1 diabetes?
Type 1 diabetes occurs when the immune system attacks the cells in the pancreas responsible for producing insulin, called beta cells. It affects less than 10% of diabetics, compared to 90% for type 2 diabetes, which is linked to a sedentary lifestyle and being overweight.
Type 1 diabetes is therefore an autoimmune disease which generally appears in children or adolescents. It is treated with insulin injections that patients must take for life.
A promising experience… but not accessible to everyone
Questioned by our colleagues from Sciences and Future, Professor Raphaël Scharfmann, researcher at Inserm and pioneer in the field of pancreatic ß cells, explains that beyond this isolated case, the treatment should not quickly be able to be generalized.
“It’s not for everyone” he believes, emphasizing that the patient presents a very particular profile. “In addition to her type 1 diabetes that appeared as a teenager, she suffers from parallel pathologies, has already had a liver and pancreas transplant and is taking immunosuppressive treatment. [pour maximiser les chances de réussite de la greffe de foie]”, explains the specialist. So it’s still unclear whether her immune system will repeat the type of attack that caused her to suffer from type 1 diabetes in the first place.
The researchers themselves say they do not know exactly why this technique finally worked in this patient but never in previous trials with other patients. However, they intend to repeat the experience, on 10 or 20 patients in total.

