Posted ,
Reading 2 mins.
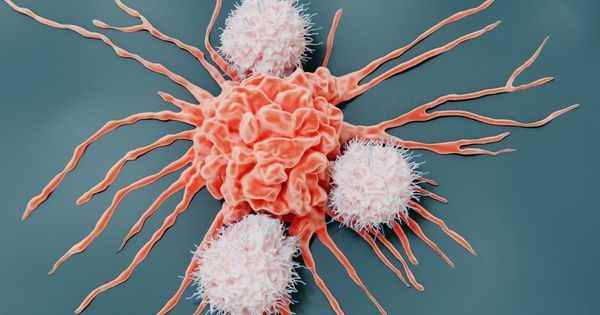
Immunotherapy has changed the treatment of many cancers but not all patients respond to it or not completely. This could change tomorrow thanks to the work of a Toulouse team which has succeeded in visualizing the path taken by killer lymphocytes to access tumors and destroy them. A major discovery.
Immunotherapy, a revolution for many cancers
A veritable therapeutic revolution for certain cancers, immunotherapy restores the capacity of the immune system to fight against tumours. By blocking the mechanism by which cancer cells blind our natural defences, these new drugs make it possible to reactivate the immune defenses and the mobilization of killer lymphocytes.
These drugs have cured some patients with metastatic melanoma (skin cancer), who were once doomed. Unfortunately, immunotherapy does not work for all patients or for all cancers.
A better understanding of the mode of action of the treatment could make it possible to improve it and make it effective in a greater number of patients. This is the goal of the team of researchers from Toulouse who lift the veil on the mechanisms that allow killer lymphocytes to penetrate tumors to destroy them.
Blood vessels identified and filmed
A team of Inserm researchers from Toulouse has just proved that particular blood vessels, baptized HEV for “High Endothelial Veinule” are the entry points for T lymphocytes to the tumour. “We have identified these HEV vessels as the gateways for lymphocytes into tumors during immunotherapy treatment, and even before treatment. We succeeded in filming, with very sophisticated microscopy techniques, these lymphocytes which roll, which stop and thread their way at the level of the vessel to enter the cancerous tumour.”explains Jean-Philippe Girard, Inserm Research Director at the Institute of Pharmacology and Structural Biology (CNRS/Toulouse III University – Paul-Sabatier) which publishes its research results in the journal Cancer Cell, February 3, 2022.
Assess response to immunotherapy treatment
To better understand also the role of T lymphocytes, the scientists conducted a clinical study with around a hundred patients suffering from melanoma. By studying the sections of tumors taken, they counted the number of small HEV vessels that were there.
And according to Professor Caroline Robert, head of the dermatology department at the Gustave-Roussy cancer treatment center in Villejuif, they observed that “when there were many HEV vessels in the metastases, the patients responded better to immunotherapy and they had a longer survival. It’s very clean. HEV vessels are really associated with the response to immunotherapy”.
True biomarkers, these vessels are able to predict whether their patients will respond well to immunotherapy treatment.
Consult an oncologist online
Boosting “HEV” vessels to improve treatment response
Another discovery by Jean-Philippe Girard’s team could prove to be a key element for access to and response to immunotherapy treatments. By succeeding in increasing the HEV vessels, they were able to demonstrate that the T lymphocytes had more access to the tumor and therefore that immunotherapy was more effective. This discovery therefore paves the way for treatments capable of improving the effectiveness of immunotherapy treatments but also of making this treatment accessible and effective in patients who today do not benefit from it!
“Our work could allow in the longer term to improve immunotherapy treatment for patients with metastatic melanoma and other types of solid tumors. They also have prognostic implications, as clinicians can now look to HEV vessels to predict a patient’s response to immunotherapy.”concludes Jean-Philippe Girard.