Published on
Updated
Reading 3 mins.
in collaboration with
Ivan Pourmir (medical oncologist)
A patient with leukemia as well as HIV was potentially cured by a stem cell transplant from cord blood, a study has found. If the patient’s skin color is mentioned here, it is because a protective genetic mutation sought in previous cases did not work on people of color.
Cord blood stem cells potentially cured the first Métis woman with HIV. The announcement of March 16 is published in the journal Cell by a team from UCLA. The good news brings in fact new information on the potential treatment of a person with HIV and cancer, here leukemia: in addition to bone marrow transplantation, cord blood also makes it possible to benefit from the necessary stem cells.
Cord blood considered to fit genetic characteristics
Last February, the Institut Pasteur announced a third proven case of HIV cure in a European also affected by leukemia, via a stem cell transplant from an anonymous donor. In this case, the researchers are looking for a compatible donor, but above all a carrier of a rare genetic mutation, CCR5 delta-32, known to prevent the entry of HIV into cells, and therefore protect against infection. However, the experience is not or hardly possible with a person of color. “The HIV epidemic is racially diverse, and it is extremely rare for people of color or race to find a sufficiently matched and unrelated adult donor”says Yvonne Bryson of UCLA, who co-led the study.
In fact, only one percent of Caucasian (white) populations today carry the CCR5-delta32 mutation and it is even rarer in other populations. This rarity limits the potential for transplanting stem cells carrying the beneficial mutation into patients of color. However, these stem cell transplants generally require a strong correspondence between the donor and the recipient.
Due to the impossibility of finding the patient an adult donor compatible with the mutation, the research team decided instead to turn to stem cells carrying CCR5-delta32 from banked umbilical cord blood in an attempt to to simultaneously cure the patient’s cancer and HIV.
Stem cells infused with those of a parent to increase the odds
To increase the chances of this rare and clinical case, banked umbilical cord blood cells were infused alongside stem cells from one of the patient’s relatives. An innovative procedure that the scientist is developing: “With cord blood, you might not have as many cells, and it takes them a bit longer to populate the body after they’re infused. Using a mixture of stem cells from a parent matched patient and cord blood cells gives cord blood cells a boost”.
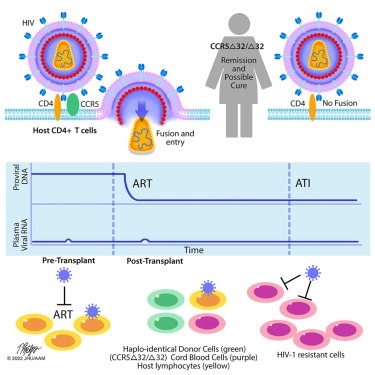
Verdict of this cord blood transplant? Thirty-seven months later, the patient was able to stop taking HIV antiviral drugs. Doctors observed that she had been HIV-negative for more than 30 months since stopping antivirals. Like the patient cured in February, the woman mentioned in this study was able to benefit from this CCR5-delta32 mutation, which is definitely at the heart of this double cure. “Stem cell transplants with CCR5-delta32/32 cells offer a two-for-one cure for people living with HIV and blood cancers” confirm the authors.
“A case that remains extremely rare”
For Doctor Ivan Pourmir, immunologist contacted by Doctissimo, the published case is very interesting, but remains for the time being an extremely rare case.
“We are counting a little on the coincidence of a treatment for leukemia which would also treat HIV, but this is not to be considered as a possible treatment on a large scale”. That said, the expert takes this notion of umbilical cord blood as a fact to be invested more : “We know thanks to these studies that stem cells carrying the mutation of the CCR5 protein are effective in making people insensitive to HIV. We also know that stem cells can allow a cell transplant in the case of leukemia, to remake the patient’s white blood cells. On the other hand, for this transplant to be effective, it must come from a person very close to the person so as not to risk a graft against host attack” he explains.
“This mutation of the CCR5 protein being more frequent in the northern European population, finding a compatible donor proved to be complicated. In this case, they found a donor, carrying this mutation, and in umbilical cord stem cells. It was the perfect combination to make the patient’s white blood cells impenetrable to HIV. But it is a solution that is difficult to generalize at the moment.
