Posted ,
Reading 3 mins.
For all diseases, the earlier the diagnosis, the more the management, whether medical or multidisciplinary, is optimized. This is also the case for autism spectrum disorder (ASD), as researcher Alpen Ortug, also lead author of the study, points out, “Earlier detection means better treatment”. This is why he and his team wanted to verify that it was possible to identify this disorder from an early age, even before birth.
Useful diagnostic tools only from 18 months
Autism spectrum disorder affects 1 in 68 children in America. According to the French system Autisme info service, the ASD, formerly known under the name TED, for Invasive Developmental Disorders, is characterized by a set of neurobiological disorders acting on the development of people called “autistic”. ASD has an impact on the social and communicative interactions of the patient, but also on their emotional awareness, their perception as well as on their behavior and activities.
Currently, the various tools for diagnosing autism can only do so around the age of 18 months. The detection of autistic disorder remains difficult because the causes are still mysterious, even if the scientific community agrees that genetic and environmental factors could favor its occurrence.
Nowadays as the High Authority for Health said, children with autism are diagnosed too late, on average between 3 and 5 years old. If the diagnosis can theoretically be made from 18 months, the situation is complex due in particular to inequalities in access to diagnosis on the territory and a lack of visibility for families who do not know which professionals to contact.
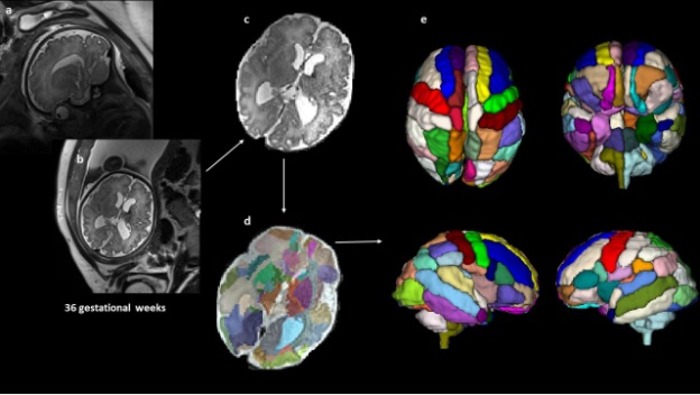
However, a study by Alpen Ortug of Harvard Medical School and presented at the Pennsylvania Medical Congress reveals the possibility of identifying ASD in-utero. Indeed, the conclusions of the study suggest that a biological marker visible through Magnetic Resonance Imaging (MRI) performed prenatally, can predict the possible emergence of ASD later in life. child.
Notable in-utero differences at the brain level
The researchers analyzed brain images given by MRI of 39 fetuses, which had been taken at around 25 weeks’ gestation, at Boston Children’s Hospital. According to their observations:
- 9 of the children were later diagnosed with ASD;
- 20 were neurotypical (neurological functioning considered normal);
- 10 did not have ASD, but other health problems, also found in children with ASD.
Secondly, the experts methodically dissected the different scans, using a technique for segmenting the brain regions between the different groups. They noted significant differences in the ASD group, particularly in the insular lobe of the brain. However, the insular cortex or insula could play a role, among other things, in the perception of oneself and others, but also in the management of emotions, decision-making and social behavior. Imaging of the TSA group showed that this insular lobe was larger than in the other groups.
In addition, the researchers noticed, in the ASD group, that the children had a larger hippocampal amygdala and commissure than in children without ASD, but suffering from other health problems. As a reminder, the cerebral hippocampus has essential functions for memory.
Consult a therapist online
What application in practice?
These results demonstrate the possibility of identifying certain markers of ASD in the uterus and at the prenatal stage. For Dr. Alpen Ortung, from Massachusetts General Hospital: “Since many genetic and environmental factors could affect the emergence of ASD from the fetal stages, it is ideal to identify the first signature of brain abnormalities in future autistic patients” from the fetal stages. And to add that it is “of the first attempt at semi-automatic segmentation of brain regions at the prenatal stage in patients who are later diagnosed with autism and [permettant] compare different control groups“.
These data on a small number of fetuses will need to be confirmed. In practice, it is hard to imagine in utero screening for autism spectrum disorders in pregnant women (unless we can clearly identify significant risks of the occurrence of this disorder in the child). But this discovery could contribute to detecting genetic or environmental factors which could explain the occurrence of this disorder and in particular its increase: from 1 case per 5,000 in the general population in 1975, we have gone to 1 per 100 today.