Published on
updated on
Reading 3 min.
Deep brain stimulation has changed the way Parkinson’s disease is treated, but some symptoms persist, particularly related to movement and sleep. American researchers have combined this technique with artificial intelligence to greatly improve the daily lives of patients.
In a small study, researchers have successfully combined deep brain stimulation with artificial intelligence systems to help Parkinson’s patients suffer fewer symptoms.
Current limitations of Parkinson’s disease treatments
Conventional treatment for Parkinson’s disease often relies on levodopa, a drug used to replace the dopamine missing from the brain due to the disease. Because the amount of the drug in the brain fluctuates, peaking shortly after the drug is given and gradually decreasing as it is metabolized by the body,
Deep brain stimulation involves implanting thin wires called electrodes into the brain at specific locations. These wires then deliver electrical signals that can help alleviate symptoms of brain disorders such as Parkinson’s disease. Conventional deep brain stimulation provides a constant level of stimulation and can also cause unwanted side effects because the brain does not always need the same intensity of treatment.
The principle of the adaptive DBS system
For several years, Professor Philip Starr and his colleagues at the University of California, San Francisco, have been looking to improve this care. In 2018, they reported the development of a adaptive DBS system called a “closed-loop” system, capable of adjusting stimulation based on data from the brain itself. Later, in 2021, they described their ability to record brain activity people in their daily lives.
By combining these two results, they succeeded in using brain activity recorded during normal daily life activities to drive the asynchronous deep brain stimulation system.
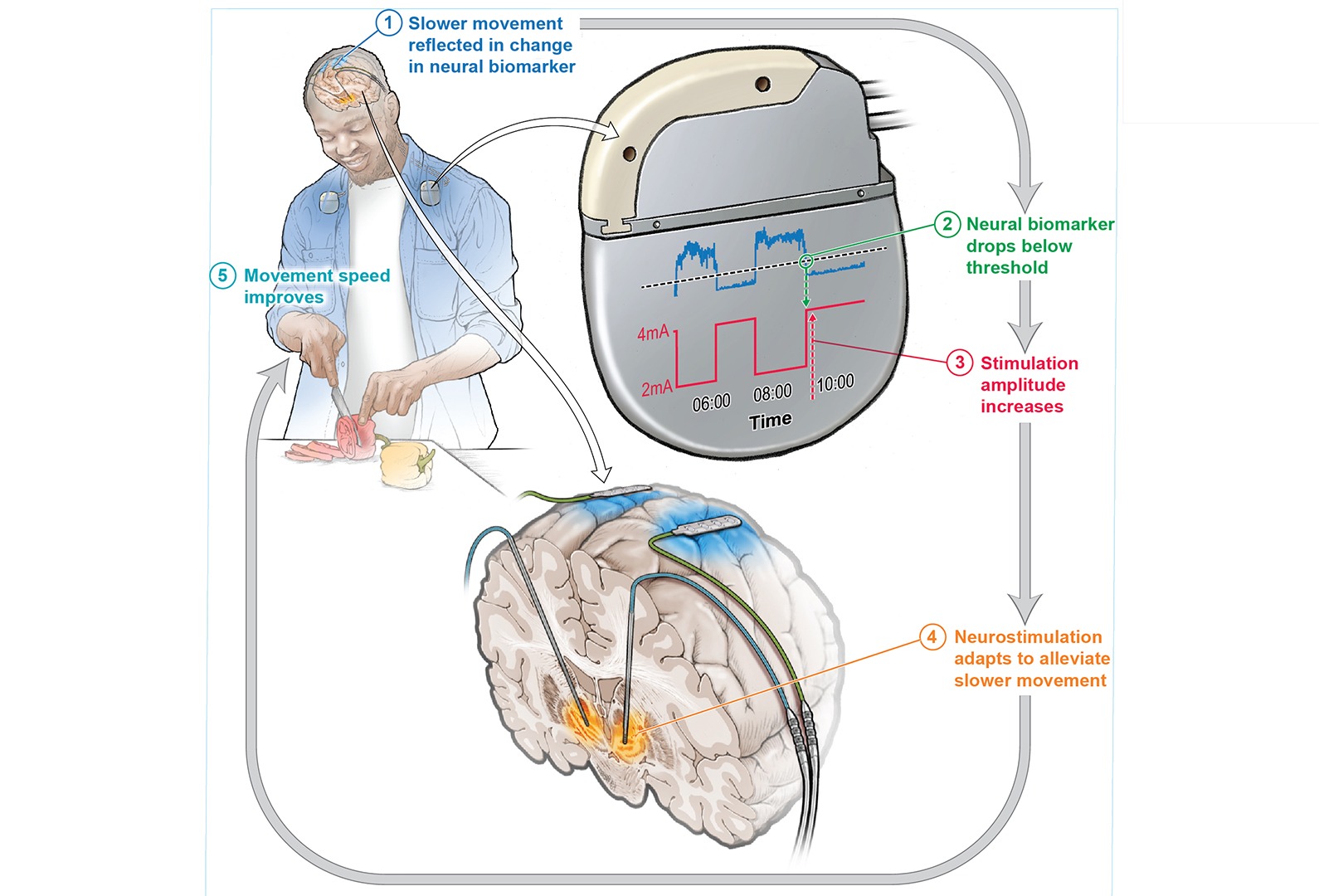
The result: Asynchronous deep brain stimulation (DBSa) uses data taken directly from a person’s brain and uses machine learning to adjust the level of stimulation in real time as the person’s needs change.The big change (…) is that we are able to detect, in real time, where a patient is on the spectrum of symptoms and match them with the exact amount of stimulation they need.” said lead author Professor Simon Little.
Halving of bothersome symptoms
In a small study, researchers asked 4 people already receiving standard DBS what they thought was the most bothersome symptom that persisted. In many cases, it was involuntary movements or difficulty initiating movement. The participants were then primed to receive the DBSa treatment. After training the DBS algorithm for several months, the participants were sent home. To compare standard DBS and DBSa, the treatment was switched between the two every two to seven days without the patients being informed.
Result: The DBSa system improved each participant’s most bothersome symptom by about 50% compared to conventional DBS. Even though they were not informed about the type of treatment they were receiving at any given time, 3 of the 4 participants were able to guess when they were benefiting from the new treatment because of the reduction in their symptoms.
Real hope even if several steps remain to be taken
Beyond these promising results, which remain to be confirmed on a larger sample, the treatment implemented today cannot be available to a large number of patients. Its implementation today requires specialized clinicians, repeated visits to adjust the settings… steps that researchers hope to be able to automate tomorrow.One of the major problems facing DBS, even in approved indications like Parkinson’s disease, is access, both for patients in terms of where they can get it and for physicians who need special training to program these devices.” said author Prof. Megan Frankowski.If there was a way for a system to find the most optimal settings at the push of a button, it would really increase the availability of this treatment to more people.“.
