Cancer of the penis (of the glans or penis) is a rare cancer that occurs in men aged 60 on average. What are the symptoms ? The risk factors? Can we cure it and what survival?
THE cancer of the penis, glans, inner face of the foreskin or penis, is a rare cancer in France. In France, the estimated number of new cases of penile cancer in 2018 was 449, says Public health France. Its average age of onset is 60 years. Its main risk factor is phimosis or lack of circumcision, associated with a lack of sufficient local hygiene and with a sexually transmitted infection by the papillomavirus (types 16 and 18). What are symptoms ? The risk factors? Can we cure it? What survival?
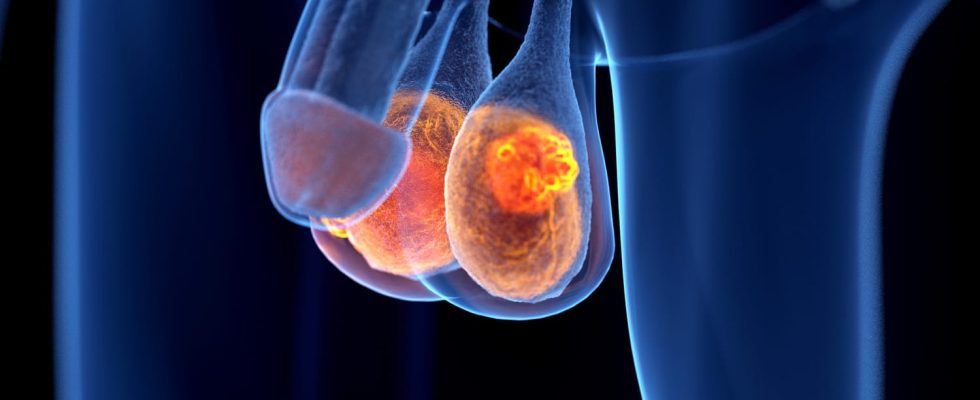
What is penile cancer?
In most cases, penile cancer presents as a skin tumor, usually a squamous cell carcinoma. Clinically, we find an induration with an ulceration at the end of the penis. Sometimes there are inguinal nodes. These lesions can bleed. They sit on:
- the glans (48%)
- the foreskin (the inner face) (21%)
- the crown (6%)
- the cavernous body (2%)
What are the chances of surviving penile cancer?
According to figures from Public Health France (2018), the standardized 5-year net survival is 68% for cases diagnosed between 2010 and 2015. Net 5-year survival decreases with age at diagnosis from 79% at age 50 to 60% at age 80.
What is the average age of penile cancer?
The age of diagnosis of penile cancer is around 60 years.
What are the symptoms of penile cancer?
The first signs of the disease are generally not specific ; this is for example a harder lump or swelling at the level of the glans or the foreskin. Penile cancer usually causes problems only in the advanced stage. The most characteristic are the following:
- a budding lesion of the glans or on the contrary ulcerated, digging
- a flow
- bleeding
What can cause penile cancer?
The lack of hygieneaggravated by the existence of a phimosis (condition of the penis) preventing any capping, increases the risk of penile cancer. “Indeed, microbial development can lead to inflammation implicated in the development of cancer, explains Dr. Ludovic Ferretti, member of the andrology and sexual medicine committee of the French Association of Urology. ATThus, we recommend a classic cleaning with water and soap after removing the cap (without forcing), then drying. And after urinating, wipe the glans well so as not to let acidic urine seep under the foreskin, which would promote inflammation.“
Which men are at risk of getting penile cancer?
There is compelling evidence that certain factors increase the risk of penile cancer. Among them :
- chronic inflammation of the penis due to poor genital hygiene
- human papillomavirus infection (HPV)
- a narrowing of the foreskinalso called phimosis : this condition prevents the foreskin from retracting to uncover the glans, which makes genital hygiene more difficult and can mask a skin lesion
- smoking
- precancerous lesions such as erythroplasia of Queyrat or Bowen’s disease.
Does circumcision promote penile cancer?
No, on the contrary,he circumcision performed in childhood provides some protection against penile cancer. HPV vaccination can also lower the risk of developing the disease.
Diagnosis of penile cancer is primarily clinical, based on palpation of the penis, tumor and inguinal lymph nodes. At the level of the glans, the clinical examination confirms the tumor, measures its size and seeks above all an extension to the cavernous bodies upstream. Only in case of diagnostic doubta biopsy of the tumor will be carried out. Penile MRI or Penile Ultrasound confirm an extension to the tunica albuginea (membrane) of the corpora cavernosa in case of doubt. These examinations are painless, but require good operator experience. “Palpation of the inguinal areas is systematic in search of palpable inguinal lymph nodes, particularly below the crease of the thigh“, continues the doctor. CT scan or MRI may be useful for detecting inguinal metastases that have gone undetected on clinical examination, particularly in obese patients
► Surgery (operation) is the main method of treatment. Circumcision can sometimes be enough, but a partial or even total removal of the penis is in principle necessary when the cancer has already spread. It is therefore important to overcome any discomfort and to consult a doctor without delay in the event of a suspicious anomaly. When the tumor has reached an advanced stage and/or has metastasized to the lymph nodes located in the groin area, the affected lymph nodes are removed as well as surrounding nodes. “The evaluation of the inguinal lymph nodes is absolutely essential in the initial management of the tumor, insists the specialist. It can be performed using the “sentinel lymph node” technique which aims to study the first lymph node relay. It has been proven that the delayed management, when a lymph node lesion appears, directly impacts overall survival.“.
► Chemotherapy can complement the treatment in case of fixed nodal metastatic disease. A clinical research protocol is underway to clarify its place in the therapeutic arsenal. Psychological support is essential in the management of penile cancer. “Preservative techniques are to be preferred in most cases, respecting a carcinological safety margin of 3 mm, with possible reconstructions allowing the preservation of function and a satisfactory cosmetic appearance by teams trained in this surgery.“, recalls Dr. Ferretti.
Usually follow-up visits start every six months and then decrease in frequency over time. The duration of the follow-up is in all cases a minimum of 5 years because 90% of recurrences are in the first 5 years of which 75% in the first 2 years.
What are the complications of penile cancer?
At the level of the penis, the sequelae are essentially psychological related to the modification of the body schema and the investment of this male organ. Complications related to treatment can be:
- of the urinary complications by narrowing of the urinary canal,
- of the sexual complications by loss of length of the penis or by insensitivity in the event of treatment by brachytherapy.
- In the inguinal areas, complications are frequent due to the particular anatomy of this region, but remain minor (most often accumulation or flow of lymph).
Thanks to Dr. Ludovic Ferretti, member of the andrology and sexual medicine committee of the AFU (French Association of Urology).
Source: Survival of people with cancer in metropolitan France 1989-2018 – Penis, Public Health France