Published on
Updated
Reading 2 mins.
Thanks to a model of ocular tissues designed by 3D bioprinting, researchers now have unlimited materials to study the genesis of age-related macular degeneration and other eye diseases. Did you say fascinating?
Did you know that researchers can now “print” cells? As surprising as it may seem, this is indeed what the research team at the National Eye Institute (NEI) in the United States is doing today: using patient stem cells, scientists are now able, via 3D bioprinting to produce ocular tissues that provide insight into diseases that can lead to blindness.
An unlimited supply of eye tissue
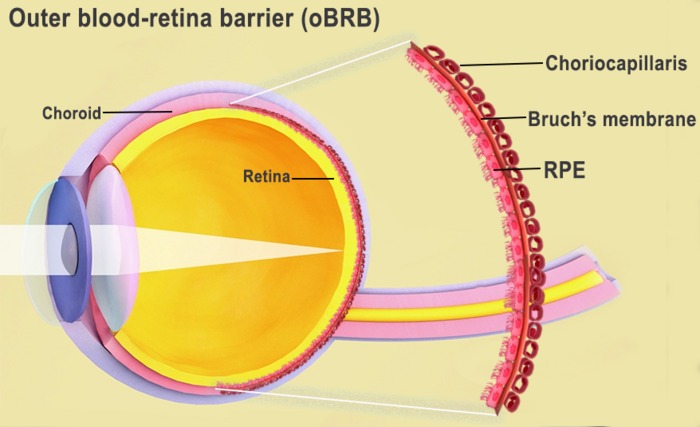
By more accurately duplicating and imprinting a combination of cells that form the outer blood-retinal barrier, an ocular tissue that supports the retina’s light-sensitive photoreceptors, this technique provides a theoretically unlimited supply of patient-derived tissue, to study the degenerative retinal diseases. An innovation that can be particularly useful, for example, in the study of age-related macular degeneration (AMD) according to a recent study. AMD is the main cause of visual impairment in the elderly.
“We know that AMD starts in the outer blood-retinal barrier”said Kapil Bharti, author of the study who leads the NEI section on eye and stem cells. “However, the mechanisms of AMD initiation and progression to the advanced dry and wet stages remain poorly understood due to the lack of physiologically relevant human models.” Thus duplicated, the cells can be better studied.
3D bioprinting to the rescue of age-related macular degeneration
The outer blood-retinal barrier is made up of the retinal pigment epithelium (RPE), separated by Bruch’s membrane from the blood vessel-rich choriocapillaris. It is this Bruch’s membrane that regulates the exchange of nutrients and waste between the choriocapillaris and the RPE. In AMD, deposits of lipoproteins form on the outside of Bruch’s membrane, impairing its function. Over time, the RPE breaks down, leading to degeneration of photoreceptors and loss of vision.
To act on this AMD, the researchers succeeded in “printing” cells. Dr. Bharti and his colleagues combined three types of immature choroidal cells in a hydrogel: pericytes, endothelial cells, which are key components of capillaries, and fibroblasts, which structure tissue. The scientists then printed the gel onto a biodegradable scaffold.
- Within days, the cells began to mature into a dense capillary network;
- On the ninth day, the scientists seeded retinal pigment epithelial cells on the back of the scaffold;
- The printed fabric reached full maturity on the 42nd day.
Results identical to native cells
Tissue analysis and genetic and functional testing showed that the imprinted tissue looked and behaved identically to the native outer blood-retinal barrier. Under induced stress, printed tissues also showed early AMD patterns – tissue degradation was also observed. Another fascinating piece of information: the drugs used to treat AMD suppressed the proliferation and migration of these vessels and restored the tissue morphology on these imprinted cells.
“Our collaborative efforts have resulted in highly relevant retinal tissue models of degenerative eye disease,” said the study’s lead author. “These tissue models have many potential uses in translational applications, including therapeutic development.”
A tremendous hope for progress which remains… to be seen.
