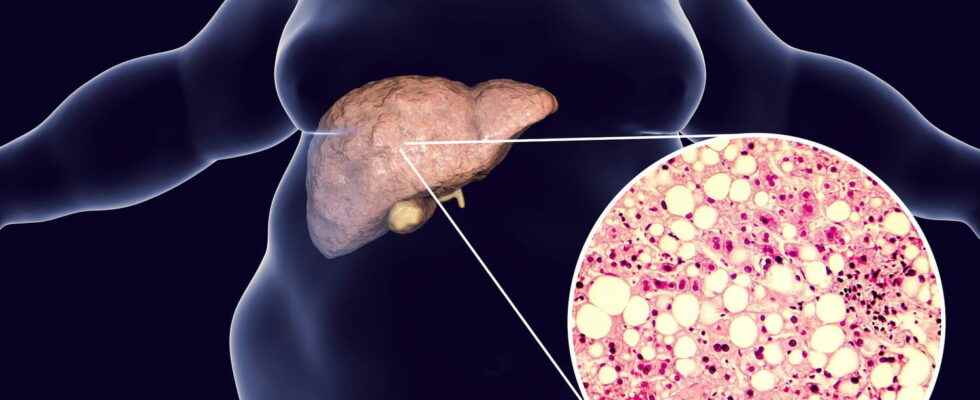
NASH (also called non-alcoholic steatohepatitis, fatty liver disease or soda) is a chronic condition of the liver. It can progress to cirrhosis or even cancer. What is this disease? What are the symptoms ? Its causes? How to treat it? Detect it with a blood test?
In France, more than 200,000 people would have severe NASH (pre-cirrhotic (just before cirrhosis) or cirrhotic stage), according to the first epidemiological investigation on the subject conducted at the national level on 100,000 participants in the Constance cohort, launched by Inserm in 2012 and whose results were published in 2020 in the journal Gastroenterology. NASH is the acronym of non-alcoholic fatty liver disease. It is also called soda disease or fatty liver disease. It is characterized by an accumulation of fat in liver cells, associated with inflammation of the liver. This disease chronic and silent liver which has long been underestimated would be more common in people who drink more than one can of sugary drink (soda …) or who smoke more than 10 cigarettes a day, reveals the study. Being imperceptible without a thorough examination, this “soda disease” or “fatty liver” can evolve, over the years, into hepatic fibrosis which itself can degenerate into cirrhosis (non-alcoholic) or liver cancer. But taken care early, it is reversible. How to spot NASH (English acronym for “non alcoholic steatohepatitis“) ? What are the risk factors? What about light products? How to treat it? Explanations and advice from Pr Patrick Marcellin, hepatologist at Beaujon Hospital and President of the APHC (Association for improving the care of patients with chronic liver disease)
Definition: what is NASH or the soda disease?
Liver is a storage organ that converts absorbed sugars into fats : fats needed for energy and brain function. This is a normal physiological mechanism of the body. Nevertheless, we are talking about steatosis when there is abnormal accumulation of fat in liver cells (called hepatocytes). “And this steatosis (which remains a warning sign whatever its stage) can become pathological when it is excessive and progressive, i.e. when there is fat overload, there are liver complications and it is associated with inflammation of the liver : this is called NASHan acronym for non-alcoholic steatohepatitis“, explains the hepatologist. Long localized in the United States and therefore unknown and underestimated in France, steatosis is more and more frequent in our country and concerns almost 1 out of 4 French people. And 20 to 30% of them would have non-alcoholic steatohepatitis, therefore NASH. Several studies have also shown that the numbers of cirrhosis, cancer and liver transplants were increasing significantly in recent years“which is obviously linked to the number of NASH on the rise“, says the specialist.
What are the symptoms of NASH?
“There are no specific symptoms related to excessive steatosis. Some people therefore suffer from NASH disease without presenting no alarming signs or particular physical manifestations“, makes a point of specifying Pr Marcellin. All the difficulty is therefore to be able to detect a NASH. Statistically, this disease mainly concerns men over 50, but also women after menopause. But in recent years, NASH has also been observed in increasingly young patients who are overweight, have an “American-style” diet (soda, lots of carbohydrates, etc.) or are unbalanced or who have certain risk factors.
What are the risk factors for NASH?
NASH could be linked to a genetic factor
This disease can affect everyone, even if there are associated risk factors. “A person who is overweight – even mild – diabetes, cholesterol, triglycerides, or high blood pressurehas a higher risk of developing NASH and must therefore be particularly vigilant“, warns the hepatologist. For the moment, we do not know very well the mechanisms responsible for inflammation or fibrosis, however, NASH could be linked to a genetic factor: “some patients would thus tend to store fat more easily in their liver and would more easily develop NASH“, explains Professor Marcellin. Research must confirm this.
What causes NASH?
Light products such as diet coke, zero .. promote steatosis
It is difficult to determine the precise causes of NASH. However, it would seem that lack of exercise, sedentary lifestyle, or a diet rich in sugars would favor the appearance of this pathology. In question : “our current dietary lifestyle (consumption of junk food, fast food, industrial products, on-the-go lunches… as well as a seated position and a sedentary lifestyle at work) means that we absorb more, even too much, sugars that can build up in the liver“, argues the expert. And you should know that sugar is linked to a phenomenon of addiction, all the more so with the effervescence of light or “zero” products which, as they contain fake sugars and sweeteners, don’t alert the brain’s satiety centers like “real sugar” would, stimulate the appetite, and trick us into consuming even more sugar. And like “the more sugars you swallow, the more you want to consume“, steatosis is becoming more and more frequent. In addition, many of the foods we eat daily do not seem to be sweet at first sight, but contain a lot of it. These are industrial products, fruit juices, sauces , sandwich loaves, dietetic products or prepared pan-fried vegetables….
To make a diagnosis of NASH, one must do a diagnosis of steatosis. Since there are no specific markers yet, people with risk factors (a little too high blood sugar with or without diabetes, a high level of fat in the blood (hyperlipidemia), mild or moderate overweight, high blood pressure…) must do :
► In a first time a blood test with a liver examination, which will detect a potentially abnormal level of transaminases. In short, “if thehe transaminases are high, this is the alarm signal of a suffering liver: it must therefore be monitored because there may be a potential steatosis or NASH“, summarizes the expert. Generally, for pure steatosis, transaminases are moderately elevated in the blood, but for NASH, transaminases are extremely elevated.
► In a second timeit will be necessary to eliminate certain causes sincea high level of transaminases may be linked to the presence of viruses in the body (remember that hepatitis B or hepatitis C raises the level of transaminases), rare diseases (drug-induced hepatitis, autoimmune hepatitis) or overconsumption of alcohol. We will then speak of alcoholic hepatitis.
► In a third time, the hepatologist will determine if it is a benign steatosis or if it is a progressive steatosis with inflammation, therefore a NASH. For this, we perform an ultrasound which will assess the amount of fat in the liver, or an elastometry (carried out usinga FibroScan®) which will make it possible to measure the amount of fat in the liver, but also to quantify fibrosis in the liver. “This examination therefore makes it possible, on the one hand, to distinguish benign steatosis from progressive steatosis associated with fibrosis, and then, on the other hand, to determine the stage of the fibrosis.“, says the expert.
Taken in time, at the pre-cirrhotic stage, the disease is reversible: a balanced diet and enough physical exercise can stop the process. Currently, there is a lot of research work on NASH: researchers are experimenting with markers that can more easily diagnose “pre-NASH”. In addition, drugs are being tested, but these have not yet proven their effectiveness: “their results are promising, but their side effects remain undetermined“, specifies the hepatologist. “So for now, there is no specific treatment to treat NASH“, apart from the liver transplant, confirms the specialist, before adding that “only the fact of change your lifestyle (eating less fat, less sugar, doing more physical activity, walking more) helps to melt liver fat and thus improve risk factors“. However, research is progressing, with several therapeutic avenues being studied:
- The CD44, a molecule present on the surface of immune cells, which participates in liver inflammation
- Kupffer cellsembryonic macrophages good for our liver
- The microbiota
It is advisable to have a multidisciplinary care and to seek the help of a nutritionist or dietitian, in addition to the hepatologist and his general practitioner. Often, weight loss is accompanied by a drop in transaminases, therefore a decrease in steatosis.
Can NASH be cured?
“Steatosis is reversible : in the absence of medication, a healthy lifestyle and a more balanced diet can reduce the risk of complications“, concludes the specialist.
Thanks to Pr Patrick Marcellin, hepatologist at Beaujon Hospital and President of the APHC (Association for the improvement of the care of patients with chronic liver diseases)